One of the challenges in medicine is that so many illnesses share the same symptoms. A plain sore throat or a cough usually isn’t a big deal. More often than not, they go away on their own. But sometimes, they’re symptoms of something more serious, like throat cancer.
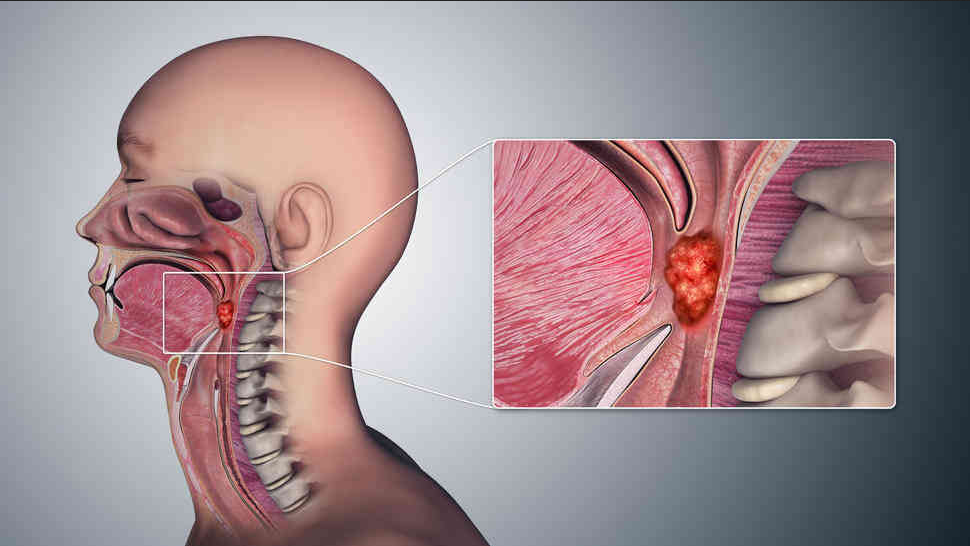
Throat cancers grow in the organs that help you swallow, speak, and breathe.
About half of these cancers happen in the throat itself, the tube that starts behind your nose and ends in your neck. It’s also called the “pharynx.” The rest start in the voice box, or “larynx.”
These diseases tend to grow quickly. That’s why getting treated early on gives you the best chance to beat them and keep a good quality of life.
Learn as much as you can so you’ll know what to expect.
You may have:
Voice changes like cracking, hoarseness, or trouble speaking clearly
Trouble swallowing or breathing
A feeling like something’s caught in your throat
A sore throat, cough (possibly with blood), or earache that won’t go away
A headache
Pain in your ears or neck
A neck lump or soreness that doesn’t go away
Unexplained weight loss
See your doctor right away if any symptoms last for more than a few weeks. But keep in mind that many conditions that aren’t cancer have these same symptoms.
You get throat cancer when some cells in your throat get a change in their genes. Doctors aren’t sure what causes this change, but these things can make it more likely:
Using tobacco for a long time. Smoking it and chewing it are the biggest risk factors for all head and neck cancers, including throat cancer.
Drinking heavily and regularly. That means more than two drinks of alcohol a day if you’re a man or more than one a day if you’re a woman.
You drive up your risk even more if you drink and you smoke.
HPV. Human papillomavirus (HPV) is linked to cancers in the back of the throat, including tongue and tonsil cancers.
You can help protect your kids from it in the future by having your children get the HPV vaccines. Kids should start the series of shots between 11 and 12 years old.
Gastroesophageal reflux disease (GERD). This chronic problem makes stomach acid flow up into your esophagus.
Other risk factors include:
Gender. Men are five times more likely to get it than women.
Age. Most people get diagnosed after 65.
Race. African American men are at the biggest risk.
Chemical exposure. This includes being around asbestos, nickel, and sulfuric acid fumes.
Diet. Not eating enough fruits and vegetables
Most types grow in the flat, thin cells that line the throat and voice box.
The two main types of throat cancer are:
Pharyngeal cancer. Your throat (pharynx) is a tube that runs from your nose to your esophagus. Your esophagus carries food from the bottom of your throat to your stomach.
Laryngeal cancer. Your voice box (larynx) sits at the bottom of your throat and contains your vocal cords.
Doctors break these groups down even further, identifying them by where they are. Pharyngeal cancer may happen in your:
Nasopharynx. This is the upper part of your throat behind your nose. In the U.S., cancer here is rare.
Oropharynx. This part is behind your mouth. Cancer is most likely to grow in the tonsils, the back of the tongue, or the soft palate (the soft area behind the roof of your mouth).
Hypopharynx. That’s the narrow area behind your voice box.
Cancer can grow in the three parts of the voice box itself. Laryngeal cancer may happen in your:
Glottis. This holds your vocal cords.
Supraglottis. This is the area above the glottis (including cancer of the epiglottis, which is like a flexible lid to your windpipe).
Subglottis. This is the area below your vocal cords and above your windpipe.
Oral sex is linked to throat cancer. There are well over 100 kinds of HPV. About 40 of them can spread if you have sexual contact with another person’s genitals, mouth, or throat. You can get oral HPV from oral sex. The infection goes away for most people in 1 or 2 years. But it doesn’t always leave your system and can cause oropharyngeal cancer years later.
Experts don’t know if having HPV alone can lead to cancer, or if you have to have another risk factor for it to happen (like being a cigarette smoker). But it causes about 70% of oropharyngeal cancer in the U.S. Cases continue to grow here, and there are more cases of throat cancer in men than cervical cancer in women – also caused by HPV.
Getting the HPV vaccine can protect you from the types of HPV that can cause throat cancer. It may prevent it. Some evidence shows that there’s possible herd immunity if enough people assigned female at birth get the vaccine. But it’s still recommended for all young people. In the U.S., 54.5% of teens ages 13 to 15 got two or three doses.
You should get the HPV vaccine if you’re:
11 to 12 years old. You should get two doses spaced 6 to 12 months apart. If you start it later, you’ll need a third dose. (Children can get the first dose as early as 9 years old.)
A young adult through 26 years old.
Over 26, maybe. It may not be as protective because you may already have been exposed to HPV. Ask your doctor.
The more sexual partners you have, the more likely you are to get throat cancer.
To prevent throat cancer:
Get the HPV vaccine.
Limit how many sexual partners you have.
Practice safe sex by using things like condoms and dental dams.
Limit how much sun you get.
Make sure your dentist checks your tonsils and tongue regularly.
Eat a healthy diet.
Limit alcohol and tobacco use.
Your doctor will examine you and ask about your general health, smoking and drinking habits, and sexual history.
They might use devices to get a closer look at your throat.
If the doctor thinks you may have cancer, they’ll order tests and procedures depending on what kind they suspect. Here are some common ones:
A biopsy collects a tissue sample that gets examined under a microscope to look for cancer cells. It’s the only way to know for sure if a tumor is cancer and what kind it is. The procedure may be done with surgery, fine needles, or an endoscope – a flexible tube with a camera that’s lowered into the throat through your nose or mouth. A tool on the end will take the biopsy.
Imaging tests can help doctors find a tumor. They can also show how big it is and if it has spread. These include:
MRI or CT scan
PET scan
X-rays
If cancer of the oropharynx is found, the sample may be tested for HPV. Usually, someone’s health outlook is better if their disease tests positive for this virus rather than being smoking-related cancer.
Each type of this cancer has its own rules for staging, which describes how severe the disease is.
But generally, stages I and II are smaller cancers and remain in one area of the organ.
Stage III diseases may have gone to lymph nodes or other parts of the throat.
And stage IV cancers may have spread to lymph nodes and different parts of the head, neck, or chest. The most serious stage IV cancers have traveled to distant parts of the body like the lungs or liver.
Doctors will try to get rid of the tumor, keep the cancer from spreading, and protect your ability to swallow and speak as much as possible.
Your treatment will depend on:
The stage of your cancer
Where it is
Your general health
Your preferences
You may have one or more treatments:
Radiation uses high-energy rays to kill cancer cells. It’s given outside your body by a machine, or inside by radioactive seeds planted near the cancer. Sometimes radiation is the only treatment needed for early-stage cancers. But it can be used with chemotherapy or surgery to treat later-stage disease.
Surgery may be done through cuts with a scalpel. It may also be less invasive – going in through the mouth with a tube called an endoscope, or with lasers or robotic techniques.
Very early cancers can usually be taken out with endoscopes or lasers.
If your cancer is more advanced, parts or all of your larynx or pharynx may need to be removed. This may affect your ability to swallow, breathe, or speak normally.
Doctors may use tissue from another spot in your body to rebuild parts of your throat to help you swallow.
If your voice box is removed, the surgeon will attach your windpipe to an opening in your neck, called a stoma, so you can breathe.
If cancer has spread deep in your neck, your surgeon may do an operation to remove lymph nodes.
Chemotherapy drugs can kill cancer and stop it from spreading. It may be used before surgery to shrink tumors, or after to keep the disease from coming back. Some chemo drugs can make radiation work better.
Targeted therapy drugs can starve cancer cells by blocking substances they need to grow.
Your doctor can prescribe medication to help you manage pain.
You may have problems during or after your treatment. Specialists can:
Show you how to care for your stoma
Teach you to speak if you have no voice box
Come up with ways to make swallowing or eating easier
Take care of yourself. Your treatment might take a lot out of you. So get enough rest, exercise when you can, and fill your plate with healthy food, like fruits and veggies.
Quit tobacco and limit alcohol. Smoking and drinking can make treatments less effective, and they raise your risk of getting another cancer.
Keep your appointments. Your doctor will follow you closely for the first few years. They’ll look for signs that the cancer has come back.